Abstract
Background: Sex differences in the outcomes of patients have been documented in several cancers including in diffuse large B-cell lymphomas (DLBCL). Men with DLBCL have been found to have poorer outcomes compared to women with rituximab-based therapy. Higher body mass index (BMI) has been found to be protective in patients with DLBCL. These sex specific differences in outcome are also more pronounced with age (Zhou JNCCN 2016; Behesthi Cancer Inform 2015). One potential mechanism that may help explain these findings are sex specific differences in metabolism. Visceral fat stores are higher in men compared to women, and increased visceral fat is associated with poorer outcomes in multiple cancers including hepatocellular cancer, pancreatic cancer, renal cell cancer, ovarian cancer and metastatic melanoma. We recently discovered that visceral obesity measured by relative visceral fat area (rVFA) using computed tomography (CT) imaging selectively stratified women, but not men, with renal cell carcinoma (Nguyen Radiology 2018). Given the prognostic value of sex in solid tumor malignancies, we sought to evaluate the prognostic value of rVFA using CT imaging in patients with DLBCL.
Methods: This is a retrospective study of consecutively treated patients diagnosed with DLBCL between 10/2006-12/2016 who were treated at the Washington University in St Louis. Patients were included if they met the following criteria: 1) a pathological diagnosis of de novo DLBCL; 2) pre-treatment CT or PET-CT available for analysis. Those with transformed DLBCL, primary Central Nervous System lymphoma, primary mediastinal B-cell lymphoma, intravascular lymphoma, gray zone lymphoma and post-transplant lymphoproliferative disease were excluded. Those with any active secondary malignancy, concurrent HIV, or patients with imaging showing more than 10% of abdominal surface area outside of the field of analysis were also excluded. Data was collected regarding baseline clinical risk factors (e.g. International Prognostic Index), cell of origin, response to therapy and clinical status. Progression-Free Survival (PFS) was defined as the time from diagnosis to relapse of disease or initiation of salvage therapy.
The patients' pre-treatment CT images were segmented into subcutaneous fat and visceral fat areas (VFAs) at the level of the umbilicus. VFA was normalized to total fat to obtain the ratio of visceral fat (rVFA) (Nguyen Radiology 2018). Optimized thresholds for identifying sex differences in PFS were obtained with Cutoff Finder (Budczies PLOS One 2012). Data was analyzed with SPSS.
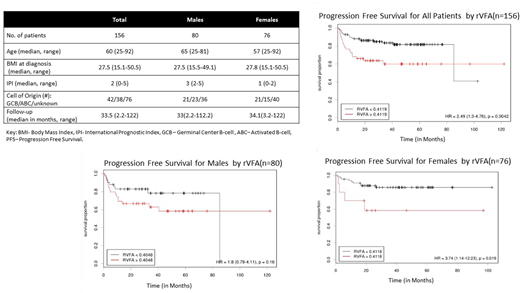
Results: 156 patients were identified (80M, 76F) with a 2-year OS of 86% and 2 year PFS 79%. Median PFS for the whole cohort was not reached. Patient characteristics are displayed on Table 1. In this cohort, median PFS was 85.2 months for men (95% CI: 22.0-147.5) and not reached for women (p=0.053). Average BMI among men and women did not differ (p=0.91). 107 (70%) patients had BMI ≥25. Those with BMI <25 had shorter median PFS (85 months; 95% CI: 2.8-167.7) compared to those with BMI ≥25 (not reached) (p=0.037). Men had a higher rVFA compared to women (0.41+0.01 vs 0.32+0.01, p<0.001). With increased age, rVFA tended to decrease in men (r=-0.22, p=0.06) but increased in women (r=0.39, p=0.0002). In all patients, an optimal rVFA threshold was established at 0.41 and those with rVFA >0.41 had higher risk of progression compared to those with rVFA <0.41 (HR 2.40, 95% CI: 1.3-4.8, p=0.004). When controlled for sex, rVFA selectively stratified women. Women with rVFA >0.41 was associated with a higher risk of progression (HR 3.70, 95% CI: 1.4-47.5, p=0.019). In contrast, no rVFA threshold could significantly risk stratify men likely to progress (HR 1.72, 95% CI: 0.77-3.85 for 0.41 threshold).
Conclusion: In this cohort of patients with diffuse large B-cell lymphoma, elevated rVFA is associated with a higher risk of progression in women with DLBCL but is not associated with worsened prognosis in men. In contrast, BMI ≥25 was associated with lower risk of progression in all patients. This recapitulates similar findings in other malignancies and suggests that sex and fat metabolism may play a role in DLBCL prognosis. Further studies should be done to evaluate these findings in a larger cohort of patients.
Mehta-Shah:Bristol-Myers Squibb: Research Funding; Celgene: Research Funding; Genetech: Research Funding; Verastem: Research Funding; Spectrum: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal